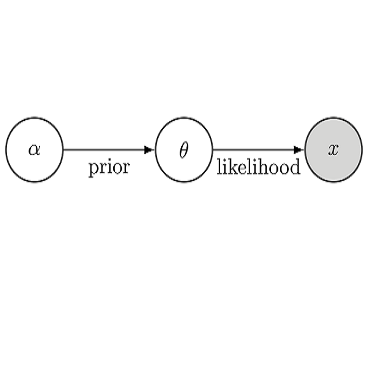
Modeling of brain tumor dynamics has the potential to advance therapeutic planning. Current modeling approaches resort to numerical solvers that simulate the tumor progression according to a given differential equation. Using highly-efficient numerical solvers, a single forward simulation takes up to a few minutes of compute. At the same time, clinical applications of tumor modeling often imply solving an inverse problem, requiring up to tens of thousands forward model evaluations when used for a Bayesian model personalization via sampling. This results in a total inference time prohibitively expensive for clinical translation. While recent data-driven approaches become capable of emulating physics simulation, they tend to fail in generalizing over the variability of the boundary conditions imposed by the patient-specific anatomy. In this paper, we propose a learnable surrogate for simulating tumor growth which maps the biophysical model parameters directly to simulation outputs, i.e. the local tumor cell densities, whilst respecting patient geometry. We test the neural solver on Bayesian tumor model personalization for a cohort of glioma patients. Bayesian inference using the proposed surrogate yields estimates analogous to those obtained by solving the forward model with a regular numerical solver. The near-real-time computation cost renders the proposed method suitable for clinical settings. The code is available at https://github.com/IvanEz/tumor-surrogate.
翻译:脑肿瘤动态模型的临床应用往往意味着解决一个反向问题,需要通过取样对巴伊西亚模型进行高达数万个前方模型评估,这导致临床翻译的推断时间过于昂贵。虽然最近的数据驱动方法能够模拟物理模拟,但它们往往无法对特定患者解剖法规定的边界条件的变异进行概括化。在本文中,我们建议为模拟结果直接绘制生物物理模型参数的模拟肿瘤生长可学习的替代模型,即当地肿瘤细胞密度,同时尊重病人的几何测量。我们测试贝伊西亚肿瘤模型的神经解析器,用于临床翻译的费用太高了。虽然最近的数据驱动方法能够模拟物理模拟,但它们往往无法对特定患者解剖法规定的边界条件的变异性进行概括。我们建议为模拟肿瘤模型设计一个可学习的替代模型,用来绘制直接模拟结果的生物模型参数,即当地肿瘤细胞密度,同时尊重病人的几何体测量。我们测试贝伊斯肿瘤模型的神经解析器,用来模拟基因组病人的个体化。Bayesianian 使用拟议的基质测算器测算出近似的模型,用来测量前方的模型。