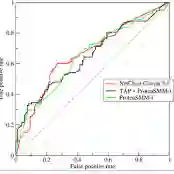
Purpose: Tumor-associated vasculature differs from healthy blood vessels by its chaotic architecture and twistedness, which promotes treatment resistance. Measurable differences in these attributes may help stratify patients by likely benefit of systemic therapy (e.g. chemotherapy). In this work, we present a new category of radiomic biomarkers called quantitative tumor-associated vasculature (QuanTAV) features, and demonstrate their ability to predict response and survival across multiple cancers, imaging modalities, and treatment regimens. Experimental Design: We segmented tumor vessels and computed mathematical measurements of twistedness and organization on routine pre-treatment radiology (CT or contrast-enhanced MRI) from 558 patients, who received one of four first-line chemotherapy-based therapeutic intervention strategies for breast (n=371) or non-small cell lung cancer (NSCLC, n=187). Results: Across 4 chemotherapy-based treatment strategies, classifiers of QuanTAV measurements significantly (p<.05) predicted response in held out testing cohorts alone (AUC=0.63-0.71) and increased AUC by 0.06-0.12 when added to models of significant clinical variables alone. QuanTAV risk scores were prognostic of recurrence free survival in treatment cohorts chemotherapy for breast cancer (p=0.002, HR=1.25, 95% CI 1.08-1.44, C-index=.66) and chemoradiation for NSCLC (p=0.039, HR=1.28, 95% CI 1.01-1.62, C-index=0.66). Categorical QuanTAV risk groups were independently prognostic among all treatment groups, including NSCLC patients receiving chemotherapy (p=0.034, HR=2.29, 95% CI 1.07-4.94, C-index=0.62). Conclusions: Across these domains, we observed an association of vascular morphology on radiology with treatment outcome. Our findings suggest the potential of tumor-associated vasculature shape and structure as a prognostic and predictive biomarker for multiple cancers and treatments.
翻译:目的:与肿瘤相关的血管特征因其混乱结构和扭曲性而不同于健康的血管,这促进了治疗抗药性。这些属性的可测量差异可能有助于通过系统治疗(例如化疗)可能受益的558名病人对病人进行分解。在这项工作中,我们展示了一个新的放射生物标志类别,称为定量肿瘤血管(QuanTAV)特征,并表明他们有能力预测多种癌症、成象模式和治疗疗程的响应和生存。实验设计:我们分解了肿瘤容器,并计算了对常规治疗前放射学(CT或对比增强的MRI)的扭曲性和组织的数学测量。 558名病人接受了四种第一线化学治疗形状(n=371)或非小细胞肺癌(NSCLC,n=187.),结果:4种基于治疗的治疗战略,这些直径直径治疗的分类,直径直径诊断结果(p.05) 仅在测试组中(AUC=0.03-0-0)直径直径直径直径,直径直径直径直径直径直径直径直径直=直径直径直径直径直径直径直径直径直位直位直位直径观察的治疗。